LAL-D should be suspected in the presence of liver and/OR lipid abnormalities without a clear CAUSE1
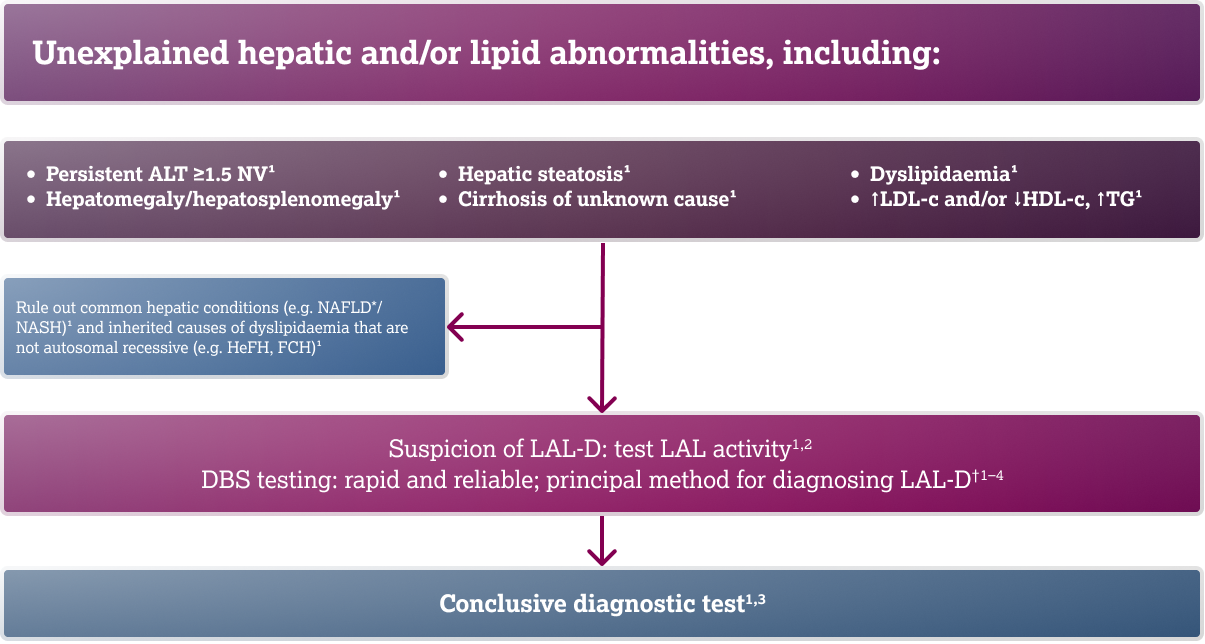
LIPA sequencing is recommended to support a diagnosis of LAL-D when a positive LAL enzyme test has been obtained1
Adapted from Camarena C, et al. 20171
and Lipiński P, et al. 2018.2
*NAFLD is now known as metabolic dysfunction-associated steatotic
liver disease (MASLD).
†LAL activity can also be assessed in leukocytes, cultured
fibroblasts, or liver tissue.1
ALT, alanine aminotransferase; DBS, dried blood spot; FCH,
familial combined hypercholesterolaemia; HDL-c, high-density
lipoprotein-cholesterol; HeFH, hereditary familial
hypercholesterolaemia; LAL, lysosomal acid lipase; LAL-D,
lysosomal acid lipase deficiency; LDL-c, low-density
lipoprotein-cholesterol; LIPA, lipase A; NAFLD, non-alcoholic
fatty liver disease; NASH, non-alcoholic steatohepatitis; NV,
normal value; TG, triglyceride.
- 1. Camarena C, et al. Med Clin (Barc). 2017;148(8):429.e1–429.e10; 2. Lipiński P, et al. J Pediatr Gastroenterol Nutr. 2018;67(4):452–457; 3. Kohli R, et al. Mol Genet Metab. 2020;129:59–66; 4. Lukacs Z, et al. Clin Chim Acta. 2017;471:201–205.
An accurate diagnosis of LAL-D is critical to inform patient management decisions1
Previous treatment approaches to managing patients with LAL-D have focused on:
*And other lipid-lowering medications.
HSCT, haemopoietic
stem cell transplant; LAL-D, lysosomal acid lipase deficiency.
-
Reiner Ž, et al. Atherosclerosis. 2014;235(1):21–30;
2. Rader DJ. N Engl J Med. 2015;373(11):1071–1073;
3. Leone L, et al. J Pediatr. 1995;127(3):509–510;
4. Kohli R, et al. Mol Genet Metab. 2020;129:59–66; - Strebinger G, et al. Hepat Med. 2019;11:79–88.
Adapted from references: 1-3
An accurate diagnosis of LAL-D is critical to inform patient management decisions1
Possible interdisciplinary team members
Adapted from references: 1-3
- Vijay S, et al. Orphanet J Rare Dis. 2021;16:13; 2. Baronio F, et al. Mol Genet Metab Rep. 2022;30:100833; 3. Kohli R, et al. Mol Genet Metab. 2020;129:59–66.