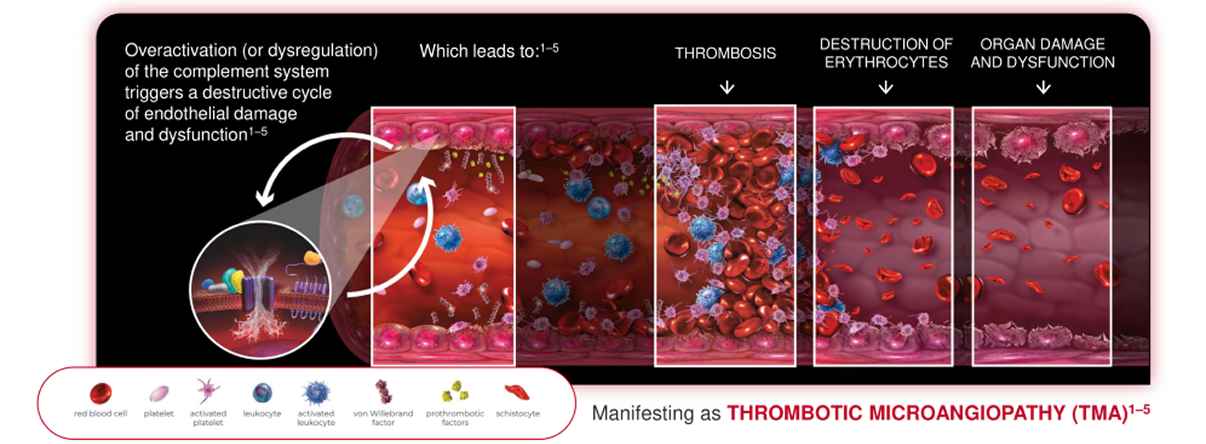
Atypical haemolyticuraemic syndrome (aHUS) is a form of thrombotic microangiopathy (TMA) caused by overactivation of the terminal complement system.1 The overactivation of the complement system triggers a destructive cycle of endothelial damage and dysfunction which leads to thrombosis, destruction of erythrocytes and organ damage and dysfunction. aHUS is a life-threatening condition and can lead to stroke, heart attack, kidney failure and premature death.1-2,4-6
In some patients, there may be no identified genetic variant; 30–50% of aHUS patients do not have an identified disease-causing genetic driver. Genetic testing is not required for a diagnosis of aHUS.2,7-10
Potential triggers include:1–5
aHUS can lead to:1–2
Gain valuable insights into spotting the disease and accessing the tools that can support efficient referral processes.
Do you know how aHUS
can be diagnosed?
Learn more
- Laurence J, et al. Clin Adv Hematol Oncol. 2016;14:2–15.
- Azoulay E, et al. Chest. 2017;152:424–434.
- Nester CM, Thomas CP. Hematology Am Soc Hematol Educ Program. 2012;2012:617–625.
- Goodship THJ, et al. Kidney Int. 2017;91:539–551.
- Bommer M, et al. Dtsch Arztebl Int. 2018;115:327–334.
- Hofer J, et al. Front Pediatr. 2014;2:97.
- Afshar-Kharghan V. Hematology Am Soc Hematol Educ Program. 2016;2016:217–225.
- Noris M, et al. Clin J Am Soc. Nephrol. 2010;5:1844–1859.
- Loirat C, et al. Pediatr. Nephrol. 2016;31(1):15-39
- Noris M, et al. Genetic atypical hemolytic-uremic syndrome. Available at:https://www.ncbi.nlm.nih.gov/books/NBK1367/
- Chatzikonstantinou T, et al. Front Med (Lausanne). 2020;7:212.
- Vande Walle J, et al. J Nephrol. 2017;30(1):127–134.